2012•04•05
Jamal Hashim, Virasakdi Chongsuvivatwong, Kai Hong Phua, Nicola Pocock, Yap Mui Teng, Rethy K. Chhem, Siswanto Agus Wilopo and Alan Lopez

UN Photo/Eskinder Debebe
Shaped by its history, geography and position as a major crossroads of trade, Southeast Asia is a region of vast social, economic and political diversity. This has contributed to the disparate health status of the region’s various populations, and to the diverse nature of its health systems, which are at varying stages of evolution. Despite their diversity, Southeast Asian countries are attempting to forge a common regional identity to seek mutually acceptable and effective solutions to key regional health challenges. This article is based on a paper from the Lancet Series on Health in Southeast Asia in which a team of researchers, including Jamal Hashim of the UNU International Institute for Global Health, presents key demographic and epidemiological changes in the region, explores the challenges facing health systems, and draws attention to the potential for regional collaboration.
• • •
Southeast Asia consists of the ten independent countries located along the continental arcs and offshore archipelagos of Asia — Brunei, Cambodia, Indonesia, Laos, Malaysia, Myanmar (Burma), the Philippines, Singapore, Thailand and Viet Nam — collectively known as the Association of Southeast Asian Nations (ASEAN). The region is home to more than half-a-billion people spread over highly diverse countries, from economic powerhouses like Singapore to poorer economies such as Cambodia, Laos and Myanmar.
In comparison with India and China, Southeast Asia is less visible in global politics and economics. The same is true of global health. We analysed the key demographic and epidemiological transitions of the region to delineate the challenges facing health systems and to emphasize the potential for regional collaboration in health. (This overview sets the scene for more detailed discussion of specific health issues in five subsequent reports in a series, profiling maternal and child health, infectious diseases, non-communicable diseases, health workforce challenges and health-care financing reforms. )
Data were gathered after a call to regional experts for information on selected subthemes related to health: geography, history, demography, epidemiology and health systems. Quantitative data were retrieved from databases of WHO, the World Bank, and the UN Population Fund, as well as from the scientific literature. Qualitative information was retrieved from grey literature (e.g., WHO reports) as well as academic literature. Data were critically appraised and analysed to elaborate trends, projections and associations between socioeconomics and population health measures.
Population and health transition
Southeast Asia contains about 600 million people, or 9 percent of the world’s population, with Indonesia having the region’s largest population (and fourth largest in the world) and Brunei the smallest.
Forty-three percent of the region’s population live in urban areas, but there is much variation between countries (from 15 percent in Cambodia to 100 percent in Singapore). Population densities range from a low of 27 people per square kilometre in Laos to a high of 7,022 per square km in Singapore. Further, although population sizes may be similar, greater sprawl can mean that cities like Manila and Jakarta are less densely populated than Mumbai and Delhi.
Although urbanization is expected to continue to rise in the region, urban slum populations seem to be less deprived than they are elsewhere, with about a quarter living in extreme shelter deprivation (defined by UN Habitat as a slum household lacking three or more of the following conditions: access to water, access to sanitation, access to secure tenure, a durable housing structure and sufficient living space).
Trends in mortality and fertility are also varied. Although life expectancy in all countries in the region has improved, there have been significant variations in the rate of progress. Most countries have enjoyed continuous rises in life expectancy since the 1950s. In some cases (Myanmar, Cambodia) political regimes and history of conflict have affected progress, as has HIV in Thailand.
Population age structures of countries in the region vary widely as a result of past differences in fertility, mortality and migration trends.
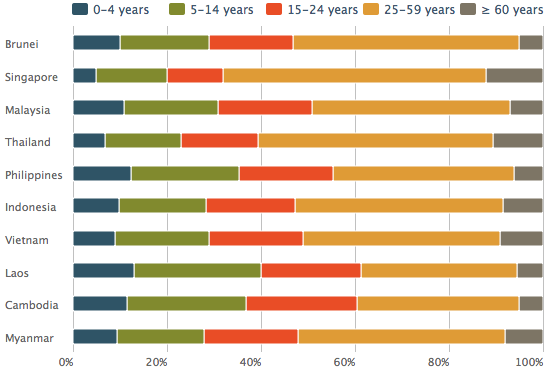
Population distribution by age in southeast Asia, 2005
These trends are, in turn, affected by economic, social, cultural and political developments. With increasing longevity, the pace of increase in numbers of the oldest old (aged 80 years and older) in Southeast Asia is projected to exceed that of East Asia over the period 2025–2050. This rise will have important implications for management of the burden of disease and healthcare provision for elderly people.
Increasing longevity is a result of diminishing burden from communicable, maternal and perinatal diseases, whereas countries with aged populations have a higher burden of noncommunicable diseases. Interestingly, mortality rates from these two groups of diseases, as well as from injuries, are correlated. Countries with high mortality rates from communicable diseases also have high death rates from chronic diseases. Deaths from communicable diseases are still prominent in Cambodia, Myanmar and Laos. Injuries are an important cause of death in all countries, though less so in Singapore and Brunei.
As countries in the region succeed in bringing communicable diseases under control, the importance of injury prevention and chronic disease control programmes will become increasingly pressing.
The region as a whole does not have reliable longitudinal data for disease trends. However, evidence from studies of disease prevalence shows a strong inverse association with national wealth, which can be largely attributed to the social determinants of health, including the provision of more efficient health systems with greater population coverage.
Regional environment and health
The environment continues to be an important contributing factor to disease and mortality in the developing world, including countries in Southeast Asia, accounting for up to a quarter of all deaths.
Southeast Asia is one of the most disaster-prone regions in the world; the Indian Ocean earthquake off the coast of Sumatra in 2004 caused a devastating tsunami in Aceh, Indonesia, and countries on the fringe of the Indian Ocean — one of the worst natural disasters ever recorded. Countries in the northern part of the region, such as the Philippines and Viet Nam, are badly affected by seasonal typhoons that have increased in intensity over time. The Philippines and Indonesia are located on the Pacific Ring of Fire, a zone prone to earthquakes and volcanoes, where around 90 percent of the world’s earthquakes occur.
Uncontrolled forest fires raged in the Indonesian states of Kalimantan and Sumatra in 1997. The severity of the fires was closely linked to the occurrence of the El Niño Southern Oscillation, which historically has brought severe drought conditions to Southeast Asia, creating conditions ripe for fires. In 1997, the gravity and extent of haze pollution was unprecedented, affecting some 300 million people across the region. The health-related cost was estimated to be US$164 million. The health effects of the 1997 haze in Southeast Asia have been well documented.
Climate change could also exacerbate the spread of emerging infectious diseases in the region, especially vector-borne diseases linked to rises in temperature and rainfall. Southeast Asia has been identified as a region that could be vulnerable to effects of climate change on health, because of large rainfall variability linked to the El Niño and La Niña oscillation, with attendant consequences for health systems.
Health systems in Southeast Asia
The pressures placed on national healthcare systems by the recent demographic and epidemiological transitions are amplified by the growing demands of an increasingly educated and affluent population for high-quality healthcare. Many traditional health practices persist alongside the use of new medical technologies and pharmaceutical products, presenting regulatory problems in terms of safety and quality.
Countries in Southeast Asia and their health system reforms can thus be categorized according to the stages of development of their healthcare systems. A typology of common issues, challenges and priorities are generated for the diverse mix of health systems at different stages of socioeconomic development.
The 1990s began with the opening up of socialist states and rapid growth among market economies in the region. Before the East Asian financial crisis in 1997–98 and the recent global economic recession, an expanding middle class in the urban populations of the larger cities pushed their demand for high-quality care into a booming private sector. As a result, market forces have turned many aspects of healthcare into a new industry in countries such as Singapore, Malaysia and Thailand, contributing to labour-force distortions for the production and distribution of health workers both within and across countries.
Following the lessons learnt from the past financial crisis, most countries have strengthened their social protection mechanisms and essential health services. Throughout the region, many innovative pro-poor financing schemes were implemented, such as the Health Card and 30-baht Schemes in Thailand, the Health Fund for the Poor in Viet Nam, Health Equity Funds in Cambodia and Laos, and, even in affluent Singapore, the Medifund, a subsidy scheme for indigent patients.
So far, the healthcare systems with dominant tax funding are fairly stable, in view of the strong role of governments and effective controls by health agencies to overcome inequity problems. However, crucial issues involve rising costs, future sustainability of centraliszd tax-financed systems, efficiency and quality of the public services, and higher public expectations.
Some of the most innovative and advanced forms of public–private mix in health services have developed within the region — for example, the restructuring or corporatization of public hospitals in Singapore from as early as 1985 and the later Swadana (self-financing) hospitals in Indonesia.
With the anticipated rise in the ageing population and future problems of intergenerational funding through pay-as-you-go mechanisms, there are experiments with new healthcare financing, such as compulsory medical savings and social insurance for long-term care. Some countries, such as the Philippines, Viet Nam and Indonesia, have radically decentralized their healthcare systems with the devolution of health services to local governments — a restructuring that has affected aspects of systems performance and equity, even though the impetus for decentralization was mainly political. Consequently, to ensure increased financial coverage and affordability, many governments have passed laws to establish national health insurance systems and mandated universal coverage, although implementation is problematic. With existing policies of decentralization and liberalization, equity issues and poor infrastructure will continue to challenge the development of the health sector.
Towards regional collaboration in global health
The severe acute respiratory syndrome (SARS) epidemic emphasized the need to strengthen regional health collaboration. This cooperation occurred via two channels: direct bilateral collaboration by individual countries (ministries of health and foreign affairs) and those under the aegis of ASEAN.
Enthusiasm for regional economic collaboration continues to grow, evident from the explicit goal of the ASEAN Free Trade Area to increase the region’s competitive advantage as a production base geared towards the world market. ASEAN leaders have identified healthcare as a priority sector for region-wide integration. From an economic perspective, opening of healthcare markets promises substantial economic gains. At the same time, however, this process could also intensify existing challenges in promotion of equitable access to healthcare within countries. It could also lead to undesirable outcomes whereby only the better-off will receive benefits from the liberalization of trade policy in health.
With globalization, ensuring accessible health services for citizens is no longer the sole responsibility of the state; healthcare in Southeast Asia is fast becoming an industry in the world market. The private sectors in Singapore, Thailand and Malaysia have capitalized on their comparative advantage to promote medical tourism and travel, combining health services for wealthy foreigners with recreational packages to boost consumption of such health services. Because of poor local economic conditions, the Philippines had a policy to export human resources for health to the world and to richer countries in the region as an income-generating mechanism. Although the financial returns from this strategy seem substantial, equity issues have surfaced concerning the negative effects of international trade in health services and workforce migration on national health systems, especially in widening disparities in the rural–urban or public–private mix.
Conclusion
Southeast Asia is a region characterized by much diversity. Social, political and economic development during the past few decades has facilitated substantial health gains in some countries, and smaller changes in others. The geology of the region, making it highly susceptible to earthquakes and resultant tsunamis, along with seasonal typhoons and floods, further increases health risks to the population from natural disasters and long-term effects of climate change. Public policy in these countries cannot ignore such risks to health, which could have important social and economic consequences. Regional cooperation around disaster preparedness and in the surveillance of and health systems response to disease outbreaks has obvious advantages as a public health strategy.
Concomitantly, all countries in the region are faced with large or looming chronic disease epidemics. Even in the poorest populations of the region, non-communicable diseases already kill more people than do communicable, maternal and perinatal conditions combined, with many of these deaths occurring before old age.
Greatly strengthened health promotion and disease prevention strategies are an urgent priority if the impressive health gains of the past few decades in most countries of the region are to be replicated. Further growth and integration of the ASEAN region should prioritize enhanced regional cooperation in the health sector to share knowledge and rationalize health systems operations, leading to further public health gains for the region’s diverse populations.
No comments:
Post a Comment